What does a life dedicated to humanitarianism look like?
Published: May 20, 2014
After graduating from the University of Toronto, James Fraser (BA 1996; MA 2001) worked with Médecins Sans Frontières / Doctors Without Borders (MSF), where the political scientist led exploratory missions and managed health care, water and community-based programs in 10 countries.
In 2003, he co-founded Dignitas International, a Toronto-based medical research organization focused on increasing access to HIV/TB treatment in low- and middle-income countries; he served as president and chief executive officer until 2012.
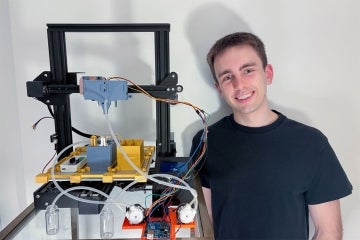
Faculty of Arts & Science writer Diana Kuprel caught up with Fraser in between trips to Africa at ChipCare, a start-up company where he is now chief executive officer. What follows is a condensed version of the interview. (Read the unabridged version.)
You’ve dedicated your academic and professional life to humanitarian work. What sparked this interest?
The spark was when I punched my brother. I grew up in Sudbury, and violence—at hockey games, watching all-night kung fu marathons with friends—was part of it and it was a caricature. I don’t really remember why, but I punched my brother in the face in front of my mom. He flew back, bloodied. My mom collapsed, wailing. I remember standing there over my brother and I had the overwhelming sense, for the first time, of what violence really is. That was the start of wanting to understand the causes of conflict, violence and suffering.
How did your university studies contribute to this journey?
I actually had a few starts, as it took me a while to figure out what I wanted to commit to. I started with Actuarial Science at U of T, because I was told it could help me earn a lot of money, and with a lack of direction that sounded like a good thing; but I didn’t like it. I went to Laurentian to study Phys Ed; but that wasn’t right either. I left school and became an ambulance attendant and a forest firefighter in Northern Ontario. The first Gulf War happened then, and I was transfixed by it. I was flipping through the U of T calendar and noticed there was a program called International Relations and another called Peace and Conflict Studies; I didn’t know you could study something like that. Those programs brought me back to U of T.
I started studying all these theories under Professor Tad Homer-Dixon and Professor Janice Stein, who were both terrific. I remember thinking, though, that what I was learning wasn’t real; it was just theory. So I did an independent study under Tad, travelling to Armenia and Azerbaijan to examine how people create enemy images. The root of violence—the ability to kill someone else—is this act of dehumanization by which one turns another person into an image of an enemy. I interviewed soldiers, refugees, humanitarian workers and academics because I wanted to figure it out for myself. It was 1994 and the Nagorno-Karabakh War—an armed conflict that was ignited when the Soviet Union collapsed—was just ending. Before the war, there were lots of intermarriages between the ethnic Armenians and Azerbaijanis in the region. At the end, each side had been basically ethnically cleansed. I wanted to figure out why. What goes through your brain when you are married to someone from the other group and a few years later you hate them all and you are ready to kill them? How does that happen within the space of a few years?
Then I did another independent study in El Salvador on its democratization process. After graduation, I was recruited by MSF.
 It takes great courage to do this kind of work. Where does that come from?
It takes great courage to do this kind of work. Where does that come from?
I don’t think of it as courage. With my brother, I saw what violence was and I was gripped by it. When I was an ambulance attendant, I tried to help people whom we couldn’t save. Once you have these kinds of experiences, it changes you. It’s hard to turn your back on something when you know it exists, and by then I knew violence and suffering existed.
It became hard to imagine a life in which I wasn’t engaged in these issues. You have one life (I think), so what is your stomach telling you to do? What are your values? These are constant companions. My mom said I’ve been having a middle age crisis since I was 18.
During your time at MSF, you worked in some of the world’s hotspots, like Colombia, Turkmenistan, Kosovo, Chechnya, Afghanistan, Sierra Leone and the Democratic Republic of Congo. Looking back to that time, what would you say is your biggest regret?
In February of 1997, I was working with MSF in Eastern Zaire (Democratic Republic of Congo). I was on an exploratory mission to set up transit camps with food, water and medical attention for refugees trying to return to Rwanda. In South Kivu, where we wanted to set up the camps, militias were trying to stop the refugees’ return by massacring them. My team and I came across a number of mass graves. Locals who helped us were later killed by the militias. We were detained and told how we would be killed and how they were going to get away with it. It was pretty intense.
On our way back out of the forest, we came across a woman lying on the side of the road. She was on her side, weak, emaciated. She had a hole in the side of her neck and I could see almost right through to the other side. Her breathing was shallow, rapid. She was dying. It was so terrible. It was like I was looking at her through a pane of glass—it was not real. No one on my team reacted.
There were some villagers nearby and we asked why they were not helping her. They said they couldn’t help the refugees because the militias had warned them that if they did, they, too, would be killed. Eventually, I grabbed some oral rehydration tablets from my bag and dropped them next to her. We got back in the vehicles and left.
Soon after leaving, I realized that no one had touched her, that I had not touched her. If I had, or if I had spoken to her, we would not have changed her fate—she still would have died—but she might have died differently, not as an animal, but as a human being. But I didn’t. Instead she died alone on the side of the road with no dignity. This is my biggest regret.
How did you come to co-found Dignitas International? It’s a huge undertaking to start up an NGO.
The question of regret actually goes to the genesis of Dignitas International. I left MSF in 2002. When my wife, Laura, and I were expecting our first child, I realized I couldn’t do the same kind of work anymore. I thought I would try to write a book on my experiences, to make sense of them, I guess. Literally, I was working on the first page when the image of the woman in Zaire who was dying on the side of the road appeared before me. I stopped writing. While I was in the field, I had seen the impact of HIV, which was devastating families and communities. The world was turning its back on the millions of people dying unnecessarily of AIDS in the developing world. It was akin to my turning my back on the woman on the side of the road. I got up, opened the door; Laura was standing there. I said we had to do something. We conspired and Dignitas was conceived. I bought a plane ticket, set up meetings in Africa to do an exploratory mission, then called a number of colleagues from MSF and we founded Dignitas.
Last year, you spoke with students at U of T’s Trudeau Centre for Peace, Conflict and Justice Studies, where you had done your undergraduate studies. What did you say to them?
I said, “You are agents of change and you can do anything. Too many Canadians wait for permission. If something in the world is bothering you, do something about it. Create a plan and work it, step by step. Don’t ask or wait for permission. Act.”
 Tell us a bit about ChipCare, the start-up founded by U of T engineers, doctors and chemists.
Tell us a bit about ChipCare, the start-up founded by U of T engineers, doctors and chemists.
We are developing a simple-to-use, extremely mobile, laboratory-quality, blood-testing platform for infectious and non-communicable diseases in low- and middle-income countries.
The brilliant ChipCare inventors have leveraged recent advances in microfluidics and biomarker technologies to make a truly revolutionary platform. The Flow-LM’s extreme mobility and simplicity of use enables community-level and mobile clinic health workers to conduct diagnostic testing in small primary care clinics, in rural health outposts and even in patients’ homes.
They will be able to perform a range of tests individually or as part of test panels for multiple diseases on a single chip. Health workers can have confidence in test results because internal and remote test validation ensures laboratory quality. And the cost of the device is significantly lower than the competition.
We have raised an investment of over $2 million from Grand Challenges Canada, Maple Leaf Angels, MaRS Innovation, Ontario Centres of Excellence and the University of Toronto. This funding will allow us to turn our bench-top prototype into a hand-held device. We expect to develop the alpha of the device by February 2015, and a sellable version by July 2015.
(Read more U of T News articles about ChipCare)
What do you see as the biggest challenge in global health today?
The biggest challenge—and it’s not a new one—is the lack of political will to make a difference. For most global health needs, the technology, diagnostics and know-how to strengthen health systems all exist. It is a question of the resources and political will to get them to the people who need it.
I have to say, with respect to HIV/AIDS, there’s been a huge change. The incidence of HIV is decreasing in many countries. Many people’s lives have been saved, and they are living with HIV as a chronic condition. And when you consider the impact of the response to HIV, not only on those people accessing treatment, but on their families, communities, schools, businesses… it is immense.
I remember when I first went into Malawi, local village chiefs spoke of Armageddon: it was all death and despair because people had no access to treatments. Society was imploding. Now it’s all changed—10 million people are now accessing lifesaving treatment globally. But 1.6 million people still died of HIV last year; another 16 million are still in need of treatment. We have a long way to go.