U of T researchers use mini-computer to remotely monitor COVID-19 patients' blood oxygen
Published: April 17, 2020
A team from the University of Toronto’s Faculty of Applied Science & Engineering has created a simple, scalable solution to remotely monitor the vital signs of COVID-19 patients, while preserving vital personal protective equipment (PPE) for health-care workers.
Currently, hospitals use a fingertip probe to monitor the respiratory status of COVID-19 patients. These probes monitor blood oxygen saturation and send the data to bedside monitors that must be read by nursing staff roughly every four hours.
But some patients experience a rapid deterioration in respiratory status that requires even more frequent monitoring, putting additional pressure on staff.
“Because health-care workers need to put on and remove PPE before interacting with patients, this requires considerable time and use of resources,” says Associate Professor Willy Wong in the Edward S. Rogers Sr. department of electrical and computer engineering and the Institute of Biomaterials and Biomedical Engineering, who led the project.
Two weeks ago, clinicians from Mount Sinai Hospital in Toronto reached out to U of T Engineering to see if researchers could come up with a solution – quickly – that would help clinicians monitor respiratory probes both continuously and remotely.
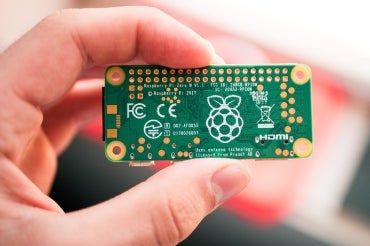
In just three days Wong and PhD candidates Bill Shi, Yan Li and Brian Wang put together a proof-of-concept using a Raspberry Pi, a simple and affordable single-board computer. Just a few days later, they were ready to deploy their prototype in a hospital setting.
“The challenge was to find something that was small, affordable and that we could put together very quickly,” says Wong. “I don’t have specific expertise in the area, but as a researcher working in the biomedical engineering group here in ECE, I have experience in the development of medical devices and thought I might be able to help.”
Raspberry Pi is a mini-computer about the size of a credit card. When attached to the fingertip probe, it can continuously read data and communicate via WiFi to a server that Wong’s team deployed.
“The most challenging part has been decoding the data the monitors provide because there are a number of different manufacturers of these probes and each one has its own format,” says Wong. “The students were working day and night to decode the data outputted from these devices.”
One key aspect is the portability of the solution that Wong and his students came up with. “In a hospital setting, we don’t really have the luxury of putting a laptop with wires going everywhere next to each patient,” says Wong. “The Raspberry Pi is something that our undergraduates use a lot in their fourth-year design projects – it just connects by cable to the oxygen saturation probe and then another cable to an outlet in the wall for power. That’s it.”
The new setup enables doctors and nurses to read a patient’s oxygen saturation levels every few minutes or less from a nursing station. The team is working with Mount Sinai and Toronto General Hospital to determine the feasibility and demand for these devices. Their solution is rapidly deployable and scalable to other venues, including emergency hospitals.
“When you put together a solution quickly, there are a few things you need to be mindful of, including concerns like patient privacy and data security, as well as usability of equipment by the front-line medical staff,” says Wong.
Wong adds that it has been a valuable experience for his students.
“This was a quintessentially electrical and computer engineering problem,” says Wong. “I saw the opportunity to help and this group of really smart and hard-working students rose to the challenge.”



