U of T researchers develop rapid MRI technique for better cancer detection and therapy

(photo by Willie B. Thomas/Getty Images)
Published: February 23, 2024
Researchers at the University of Toronto’s Faculty of Applied Science & Engineering have developed a rapid magnetic resonance imaging (MRI) technique to help doctors better detect and diagnose tumours.
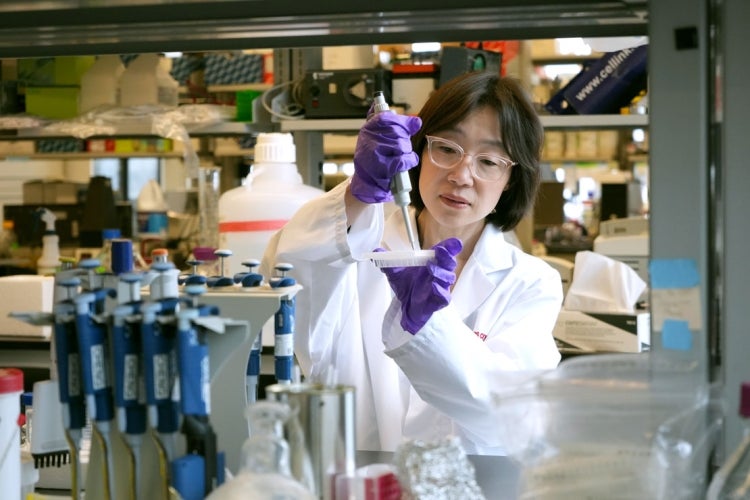
The new approach – by Hai-Ling Cheng, a professor in the Institute of Biomedical Engineering and the Edward S. Rogers Sr. department of electrical and computer engineering, and PhD candidate Alex Mertens – could provide physicians with guidance during surgery and other therapeutic interventions.
Based on novel analysis of raw patient data collected from imaging sessions with standard MRI equipment, the algorithm Cheng and Mertens developed reduces the duration between each image acquisition from more than 20 seconds to one second without sacrificing image sharpness.
“People in the field have been trying to get high spatial resolution concurrently with temporal resolution for the past 25 years,” says Cheng.
Cheng and Mertens, with the help of the U of T Innovations and Partnerships Office, have applied for a patent and are partnering with companies to bring their MRI technique to market.
“In practice, doctors always follow up imaging results with a biopsy for definitive confirmation to more accurately determine the grade of cancer and its stage,” Cheng says.
“Our technique is not meant to displace the biopsy. But by better characterizing the underlying pathology at the vascular and cellular level, we can mitigate randomness in the sampling when the doctor goes in with a biopsy needle.”
MRI is used to scan soft tissues like muscle or fat because it offers the best contrast compared to other modalities such as X-rays and ultrasounds. The contrast allows doctors to discern different cell types and identify small cancerous growths.
“Let’s say you’ve got a liver and a kidney, and you want to image them both in the same area of the body,” says Cheng. “If you were to take an X-ray, you would get one contrast level – one grey scale specific to the liver and one grey scale specific to the kidney.”
With MRI technology, however, there’s different physics at play that allows for refined gradients. An MRI scanner produces a strongly magnetized field inside the patient’s body into which it pulses a radio frequency, or RF, wave. The wave affects the water protons in soft tissues, which react to the pulse and emit signature return signals.
“The data from the return signal doesn’t tell you the shape of an object but the frequency content of the object,” says Cheng. “We structure that return RF signal into a matrix, which we can then convert into a high resolution image.”
Researchers can change the magnetic strength and the frequency of the pulse to obtain different contrasts, much like a music producer can increase and decrease the volume of individual tracks in a song.
To enhance the RF signal further, a contrast agent is intravenously injected into the patient beforehand: usually gadolinium, which is non-radioactive. The dynamics of the gadolinium distribution – that is, the speed of its uptake and washout in cells – give doctors additional information about the malignancy of the tumour.
“Tumours not only have a larger blood volume, but because their blood vessels are very messed up and tortuous, they also tend to be very, very leaky,” says Cheng.
However, the MRI procedure is notoriously slow. The scanner must repeatedly acquire frequency domain data at different coarse and fine-grain resolutions. Typical temporal resolution is 20 seconds and gadolinium washout in a tumour can take as little as 10 seconds.
“Typically, it takes 256 acquisition lines to create one image,” says Cheng. “Rather than reconstructing a full image every 20 seconds or every minute – that’s kind of pointless, because you’re missing the dynamics – our algorithm extrapolates information based on successive sampling of just one acquisition line.
“We create images every second, and sometimes less, and those images are not going to suffer from low resolution.”
“The work that Hai-Ling and her team are doing is a testament to how electrical and computer engineering technologies can impact the health-care sector,” says Professor Deepa Kundur, chair of the electrical and computer engineering department in the Faculty of Applied Science & Engineering. “Hai-Ling and Alex have spent years building on their knowledge of MRI physics and human biology, demonstrating how interdisciplinary perspectives in engineering save lives. Well done.”



