Fragmented sleep may affect brain’s immune cells, impair cognition: U of T study

Published: December 12, 2019
Fragmented sleep in older people with and without Alzheimer’s disease may have an effect on the brain’s immune cells and impact people’s cognitive abilities, according to a new study by University of Toronto researchers.
The study by Dr. Andrew Lim, an associate professor in neurology at U of T’s Faculty of Medicine, and Kirusanthy Kaneshwaran, a third-year U of T medical student, was published this week in Science Advances. It shows that in adults with fragmented sleep – where people were waking up repeatedly instead of sleeping soundly – there was an effect on microglia, and the cells showed signs of accelerated aging and other abnormalities.
The researchers were then able to identify that the changes in the microglia, described by Lim as the “brain’s innate immune cells,” could be associated with worse cognition in older adults, both with and without Alzheimer’s disease.
“There are two important takeaways from this paper,” says Lim. “One is that poor sleep is associated with brain immune dysregulation or dysfunction. The second part is that dysfunction appears to be further associated with impaired cognition.”
The research in the paper supports the hypothesis “that poor sleep may lead to brain immune dysregulation,” adds Lim, who is also a scientist at the Hurvitz Brain Sciences Research Program at Sunnybrook Research Institute.
It also supports the idea that poor sleep may be a possible cause of cognitive decline and dementia.
“Greater expression of genes characteristic of aged microglia was associated with worse cognition and partially accounted for the association between sleep fragmentation and worse cognition,” write the researchers.
“These findings raise the possibility that microglial aging and activation may be a consequence of sleep fragmentation and may link sleep fragmentation to poor cognition in older adults.”
The paper points to other potential factors that lead to cognitive impairment.
“Our findings are compatible with three scenarios: microglial aging and activation may lead to sleep fragmentation, sleep fragmentation may lead to microglial aging and activation, or both may be caused by other brain changes, such as dementia-related brain pathologies,” the researchers write.
The research was based on 685 adults who were more than 65 years old, including more than 260 who had Alzheimer’s disease.
The adults had been participants in the Religious Orders Study and Rush Memory and Aging Project.
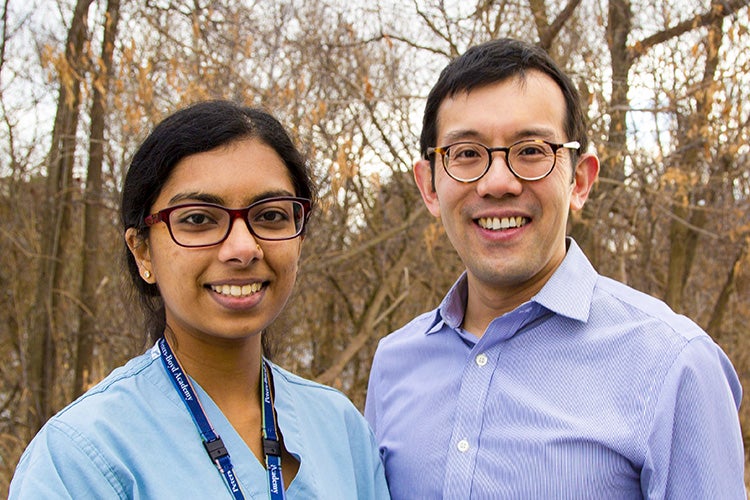
The study was undertaken by Dr. Andrew Lim, an associate professor in neurology in U of T’s Faculty of Medicine, and Kirusanthy Kaneshwaran, a third-year U of T medical student (photo by Gabrielle Giroday)
For the study, researchers measured the participants’ sleep patterns using wearable devices. They also measured participants’ cognitive function on an annual basis.
Researchers quantified the number and state of the brain’s innate immune cells for each participant by examining the gene expression patterns of the cells and by looking at the cells’ shape under the microscope.
“I have a relative with Alzheimer’s disease and I have always been fascinated about memory and what is the underlying mechanism of memory,” says Kaneshwaran, the first author of the study.
“Sleep is something that a lot of people have problems with. Losing your memory is something very deep – it’s like losing yourself as a person. I feel like it’s very important that if we can prevent that in any way, we do.”
The findings emphasize the importance of getting a good night’s rest, according to Lim.
“Poor sleep is not something that should be ignored. It should be something that is taken seriously, and pursued,” he says.
“If you are sleeping poorly, you should bring it up with your doctor. If you need to, you can then can bring it up with a sleep specialist and do the appropriate testing, and try to solve the problem. Improving sleep might potentially be a way of improving brain immune function, which may potentially improve cognition.”
Lim adds that there are promising research implications from the study.
For example, further research may target brain immune dysregulation as a way of preventing unfavourable impacts on brain health for people with unavoidable sleep disruption, including shift workers or airline workers.
The researchers received support from the Canadian Institutes of Health Research, among others.



